- Find a DoctorDoctors by Specialty
- Cardiac Electrophysiology
- Cardiology
- Colon & Rectal Surgery
- Family Medicine
- Gastroenterology
- General & Vascular Surgery
- Gynecological Oncology
- Gynecology
- Infectious Disease
- Internal Medicine
- Interventional Cardiology
- Interventional Radiology
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics & Gynecology
- Oncology
- Oncology & Hematology
- Orthopedic Surgery
- Otolaryngology
- Perinatology
- Psychiatry
- Pulmonary Medicine
- Radiation Oncology
- Rheumatology
- Sleep Medicine
- Thoracic Surgery
- Urology
- View All Doctors
- Our ServicesMedical Services
- Bariatric Services
- Behavioral & Mental Health
- Breast Care
- Cancer Care
- Critical Care
- Ear, Nose, & Throat
- Emergency Services
- Gastroenterology
- Glossary
- Heart Care
- Home Care
- Hospice & Palliative Care
- Imaging & Diagnostics
- Long-Term Care
- Nephrology
- Orthopedics
- Primary Care
- Rehabilitation Therapies
- Robotic-Assisted Surgery
- Sleep Services
- Spine Care
- Stroke Care
- Surgery Services
- Telehealth Services
- Urology
- Urgent Care
- Virtual Urgent Care
- Women’s Services
- Wound Care
- Our Locations
- Patients & Visitors
- About Us
LeConte’s Healthy Lifestyles is a health and wellness publication printed twice a month in local newspapers serving Sevier County and South Knoxville. And here online! We hope you find this information healthful.
Table of Contents
Battle of the Bulge
Hiatal Hernia Causes and Treatment
Are Hernias Preventable?
Going Against the ‘Graine
Migraines and Children
LeConte Volunteer Services Department Awards Scholarships
Chet Ramsey Receives Covenant Health’s Buscetta Award
Download this edition
Battle of the Bulge
Despite Easy Fix, Many Wait Until It’s a Hernia Emergency
 It was once considered major surgery, but today it’s among the most common surgeries around. Yet it’s rare that Jeffrey King, MD, general surgeon with LeConte Surgical Associates at LeConte Medical Center, doesn’t see at least a handful of patients a year in need of emergency hernia repair.
It was once considered major surgery, but today it’s among the most common surgeries around. Yet it’s rare that Jeffrey King, MD, general surgeon with LeConte Surgical Associates at LeConte Medical Center, doesn’t see at least a handful of patients a year in need of emergency hernia repair.
“If you have increasing pain to the area, firmness to the contents, abdominal distension, nausea, vomiting and lastly, redness around it, definitely you have waited too long,” said Dr. King.
A hernia, of course, is simply a bulging protrusion of part of an organ through the muscle wall that surrounds it. Hernias are found most often in the groin (inguinal), stomach and esophagus (hiatal), umbilical area (belly button) or around a recent surgery site (incisional).
With almost 700,000 hernia operations performed annually, it’s clear that hernias are quite common. About 10 percent of the population develops some kind of hernia during their lifetime. Men are particularly susceptible to hernias, and age and injury are common causes.
“With hernia patients, the age is distributed across all ages, from teenagers all the way up into the 80s,” said Dr. King. “Basically, most people who have symptoms want them fixed. Some people come immediately when they injure themselves at work or notice a pain in the area followed by a bulge, whereas other people have more indolent symptoms that occur over a period of time— they’ve had the bulge for multiple years and it just continually gets larger and then becomes symptomatic.”
So when should you see your doctor about a hernia? The aforementioned symptoms aside, Dr. King said “the sooner the better.”
“One thing for certain is when a defect occurs initially, it may be a small defect, there is less tissue injury and destruction, and it’s easier to repair,” said Dr. King. “As time goes on, the pressure and the contents protruding out the inguinal defect or the incisional hernia defect then begin to get expanded or enlarged. The hernia gradually gets larger and larger and becomes a larger defect to repair. There is also a higher risk of recurrence and a more difficult recovery. Most of the time it’s not an emergency, but there are times when it is an emergency.”
One of those times is when a hernia becomes “incarcerated” or “strangulated.” An incarcerated hernia is when a loop of a bowel becomes blocked or occluded, preventing solids to pass. When the hernia traps the intestine so tightly that it cuts off the blood supply, it’s a potentially life-threatening condition called strangulation. If that happens, the trapped intestine can develop gangrene in as few as six hours, killing the intestinal wall and rupturing, leading to peritonitis, shock and death if untreated.
Usually a quick, simple surgery is used to combat this “battle of the bulge” (which is what a hernia looks like).

“I don’t think an inguinal hernia poses any kind of challenge to a well-trained general surgeon,” said Dr. King. “On a complexity scale of one to 10 in surgical problem-solving and decision-making, inguinal hernias are a one. Incisional hernias get more difficult to understand how to manage correctly, and that can get into a three, four or five out of 10 difficulty range. An inguinal hernia repair has a very low morbidity, very low risk and very positive outcomes.”
Since the first recorded hernia repair took place in 1887, the technique began evolving quickly through the 1950s and 1960s. At that time, surgeons repaired the tissue by suturing structures together over the defect. In the 1970s and 1980s, however, surgeons began using mesh made of polypropylene, polyester and GoreTex. Those advancements led to lower recurrence rates, less pain and less disability.
“I think the most important thing is recognition that you have a hernia, and understanding that early intervention means recovery and definitive correction or repair of the hernia is at its highest probability,” said Dr. King. “Waiting for a defect to get repaired means it will get larger with time, the surgery to fix it will be more complicated and recovery will likely be more complicated.”
Hiatal Hernia Causes and Treatment
The cause of a hiatal hernia is unknown, but possible triggers include the following:
- Coughing
- Vomiting
- Straining during bowel movement
- Sudden physical exertion
- Pregnancy
- Obesity
Although hiatal hernias usually do not require treatment, treatment may be necessary if the hernia is:
- In danger of becoming strangulated (twisted in a way that cuts off blood supply to the stomach).
- Complicated by severe gastroesophageal reflux disease (GERD).
- Complicated by esophagitis (inflammation of the esophagus).
Medication may be prescribed by a doctor to neutralize stomach acid, decrease acid production, or strengthen the lower esophageal sphincter. The esophageal sphincter is the muscle that prevents stomach acid from coming up into the esophagus. Surgery may also be needed in these cases to reduce the size of the hernia, or to prevent strangulation by closing the opening in the diaphragm.
Are Hernias Preventable?
Will you be lucky enough to be one who escapes the seeming inevitability of a hernia? To find out, you’d probably need to take a close look inside.
That’s because hernias are ultimately caused by a weak spot in the abdomen wall. You may have been born with the weak area, or it may have become weakened by age or surgery.
“Proper lifting techniques and maintaining a healthy lifestyle in which you don’t become obese over the years is most important, but outside of that, there isn’t much that can be done,” said Jeffrey King, MD, general surgeon with LeConte Surgical Associates at LeConte Medical Center in Sevierville.
“Many people are pre-disposed for inguinal hernias or umbilical hernias because there are just natural weak spots on the abdominal wall. Of course, the complexity of incisional hernias is related to the fact that someone has already had an operation in the past and that creates weak spots along the abdominal wall.”
The best way to avoid a hernia is to reduce the pressure on those “weak spots.” In addition, to avoid obesity and take precautions when lifting, try these suggestions:
- Eat high-fiber foods with plenty of whole grains, fruits and vegetables to prevent constipation and straining with bowel movements.
- Drink plenty of water. Ask a doctor about using a stool softener.
- Stop smoking, because the accompanying cough can make a hernia worse.
- Control allergies to avoid sneezing in excess.
- Strengthen your abdominal muscles with exercise.
Going Against the ‘Graine
Understanding Why Migraines Are Not Just Headaches
The National Headache Foundation estimates that 28 million Americans suffer from migraines. More women than men get migraines, and a quarter of all women with migraines suffer four or more attacks a month, with 40 percent experiencing one or less than one severe attack a month. Each migraine can last from four hours to three days. Occasionally, it will last longer.
So what are migraine headaches?
 “This throbbing type of headache is distinguished by the fact that symptoms other than pain occur with the headache,” explains Amy Greene, nurse practitioner with Great Smokies Family Medicine. “Many people commonly experience nausea and vomiting, lightheadedness, sensitivity to light (photophobia), and other visual disturbances. Migraines are also unique in that they have distinct phases. Not all individuals experience each phase, however.”
“This throbbing type of headache is distinguished by the fact that symptoms other than pain occur with the headache,” explains Amy Greene, nurse practitioner with Great Smokies Family Medicine. “Many people commonly experience nausea and vomiting, lightheadedness, sensitivity to light (photophobia), and other visual disturbances. Migraines are also unique in that they have distinct phases. Not all individuals experience each phase, however.”
The phases of a migraine headache may include:
Premonition phase. A change in mood or behavior that may occur hours or days before the headache.
Aura phase. A group of visual, sensory, or motor symptoms that immediately precede the headache. Examples include hallucinations, numbness, changes in speech, and muscle weakness.
Headache phase. The period during the actual headache. Throbbing pain occurs on one or both sides of the head. Sensitivity to light and motion is common, as are depression, fatigue, and anxiety.
Headache resolution phase. Pain lessens during this phase, but may be replaced with fatigue, irritability, and difficulty concentrating. Some individuals feel refreshed after an attack, while others do not.
“It is important for us to try and classify a patient’s migraine to help determine the best treatment for that individual,” said Greene.
Migraines may be classified as with or without aura. Migraines with aura are experienced by fewer sufferers. Aura symptoms may include flashing light or zigzag lines, which usually appear within 30 minutes before an attack. The more common type of migraine does not include an aura phase.
How are migraines diagnosed?
“We diagnose migraine headaches based on reported symptoms, but a thorough medical exam, which may include other tests or procedures, may be used to rule out underlying diseases or conditions,” explains Greene.
Tracking and sharing information about your headache with your doctor helps with the process of making an accurate diagnosis. Consider writing down the following information to take to your medical appointment:
- Time of day when your headaches occur
- Specific location of your headaches
- How your headaches feel
- How long your headaches last
- Any changes in behavior or personality
- Effect of changes in position or activities on the headache
- Effect of headaches on sleep patterns
- Information about stress in your life
- Information about any head trauma
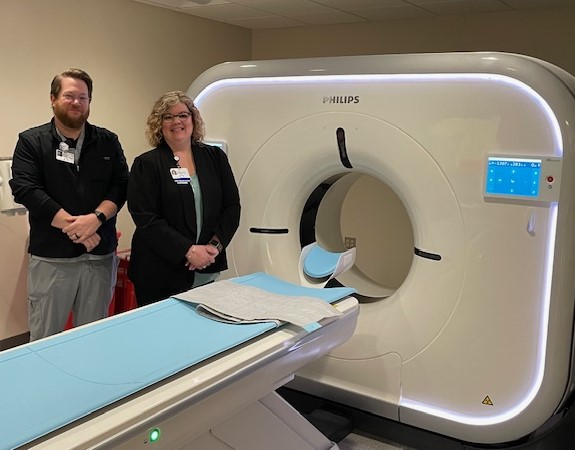
Diagnostic tests that may be used to confirm a migraine diagnosis include computerized tomography (CT) scans, magnetic resonance imagining (MRI), and spinal tap (lumbar puncture). These tests help rule out other problems, such as tumors, infection, or blood vessel irregularities that may cause migraine-like symptoms.
What is the treatment for migraines?
“Once we have narrowed down the migraine classification, specific treatment for headaches will be determined based on several factors, such as age, overall health, medical history, severity and frequency of the migraine,” says Greene. “The ultimate goal of treatment is to stop migraines from occurring.”
Migraine headache management may include:
- Avoiding known triggers, such as certain foods and beverages, lack of sleep, and fasting
- Changing eating habits
- Exercise
- Resting in a quiet, dark environment
- Medications, as recommended by your doctor
- Stress management
Migraine headaches may require specific medication management including:
Abortive medications. Medications prescribed by your doctor that act on specific receptors in both the brain and the blood vessels in the head, stopping a headache once it is in progress.
Rescue medications. Medications purchased over the counter, such as analgesics (pain relievers), to diminish or stop the headache.
Preventive medications. Medications prescribed by your doctor that are taken daily to suppress the onset of severe migraine headaches.
“Some headaches may require immediate medical attention, including hospitalization for observation, diagnostic testing, or even surgery. Treatment is individualized, depending on the underlying condition causing the headache. Full recovery depends on the type of headache and other medical problems that may be present,” explains Greene.
Migraines and Children
It’s More Common Than You May Think
 Kids get headaches and migraines, too. In fact, 20 percent of adults who suffer from headaches say their headaches started before age 10, while 50 percent say they started getting headaches before age 20.
Kids get headaches and migraines, too. In fact, 20 percent of adults who suffer from headaches say their headaches started before age 10, while 50 percent say they started getting headaches before age 20.
How Common Are Headaches in Children and Adolescents?
Headaches are very common in children and adolescents. In one study, 56 percent of boys and 74 percent of girls between the ages of 12 and 17 reported having had a headache within the past month. By age 15, 5 percent of all children and adolescents have had migraines and 15 percent have had tension headaches.
Many parents worry that their child’s headache is the sign of a brain tumor or serious medical condition, but most headaches in children and adolescents are not the result of a serious illness.
What Types of Headaches Do Children and Adolescents Get?
Children get the same types of headaches adults do, including tension headaches, migraines, and sinus headaches.
What Causes Headaches in Children and Adolescents?
Most headaches in children are due to an illness, infection, cold, or fever. Other conditions that can cause headaches include sinusitis (inflammation of the sinuses), pharyngitis (inflammation or infection of the throat), or otitis (ear infection).
Most children and adolescents—an estimated 70 percent—who have migraines have an immediate family member who also suffers from them or who did in childhood. Children and adolescents with migraines may also inherit the tendency to be affected by certain migraine triggers, such as fatigue, bright lights, and changes in weather.
Other migraine triggers can be stress, anxiety, depression, a change in routine or sleep pattern, loud noises, or certain foods, food additives, and beverages. Too much physical activity or too much sun can trigger a migraine in some children or adolescents. In girls, changes during the menstrual cycle may trigger a bad headache.
How Are Headaches Evaluated and Diagnosed in Children and Adolescents?
The good news for pediatric and adolescent headache sufferers is that once a correct headache diagnosis is made, an effective treatment plan can be started.
If your child has headache symptoms, the first step is to take your child to his or her doctor. The doctor will perform a complete physical exam and a headache evaluation. During the headache evaluation, your child’s headache history and description of the headaches will be evaluated. You and your child will be asked to describe the headache symptoms and characteristics as completely as possible.
A headache evaluation may include a CT scan or MRI if a structural disorder of the central nervous system is suspected. Both of these tests produce cross-sectional images of the brain that can reveal abnormal areas or problems.
If your child’s headache symptoms become worse or become more frequent despite treatment, he or she should be referred to a pediatric neurologist or to a headache specialist if an adolescent. Your child’s doctor should be able to provide the names of headache specialists.
How Are Headaches Treated in Children and Adolescents?
Your doctor may recommend different types of headache treatment.
The proper treatment will depend on several factors, including the type and frequency of the headache, its cause, and the age of the child. Treatment may include education, stress management, biofeedback and medications.
Stress management: To successfully treat tension headaches, it is important for kids and their parents to identify what causes or triggers the headaches. Then they can learn ways to cope or remove the stressful activities or events.
Biofeedback: Biofeedback equipment includes sensors connected to the body to monitor your child’s involuntary physical responses to headaches, such as breathing, pulse, heart rate, temperature, muscle tension, and brain activity. By learning to recognize these physical reactions and how the body responds in stressful situations, biofeedback can help your child learn how to release and control tension that causes headaches.
Medications: There are three categories of headache medications for children, including symptomatic relief, abortive, and preventive medications. Many of the drugs used to treat adult headaches are used in smaller doses to treat headaches in children and adolescents. But aspirin should not be used to treat headaches in children under age 15. Aspirin can cause Reye’s syndrome, a rare but fatal condition young kids can get.
LeConte Volunteer Services Department Awards Scholarships
[bs_row class=”row”][bs_col class=”col-sm-6″]

[/bs_col][bs_col class=”col-sm-6″]

[/bs_col][/bs_row]
[bs_row class=”row”][bs_col class=”col-sm-6″]

[/bs_col][bs_col class=”col-sm-6″]

[/bs_col][/bs_row]
[bs_row class=”row”][bs_col class=”col-sm-6″]

[/bs_col][bs_col class=”col-sm-6″]
Top left, Zach Arwood; Top right, Katlyn Laymon; Center left, Devin Narwani; Center right, Hannah Williams; Bottom, Maria Billings.
Scholarship recipients are pictured with members of the scholarship committee Julia Householder and Bob Clements.
[/bs_col][/bs_row]
The Volunteer Scholarship Committee at LeConte Medical Center selected a group of very deserving individuals to receive funds this year. The criteria to apply for the scholarship are that individuals must be volunteers, full-time employees, or children of full-time employees who are pursuing an education in a healthcare. The applicants must maintain an ideal GPA, and provide a letter of reference.
Zach Arwood has been awarded a $1000 scholarship to ETSU. He is a current volunteer in our Emergency Department, and is the son of Karen Arwood in the Pharmacy.
Katlyn Laymon has been awarded a $1000 scholarship to Tennessee Tech. She is a volunteer in the Pharmacy.
Devin Narwani has been awarded a $1000 scholarship to ETSU. He is a current hospital volunteer in multiple departments.
Hannah Williams has been awarded a $1000 scholarship to Tennessee Tech. Hannah is a current volunteer.
Mariah Billings has been awarded $500 to the University of Tennessee. She is a previous scholarship recipient, and a hospital volunteer.
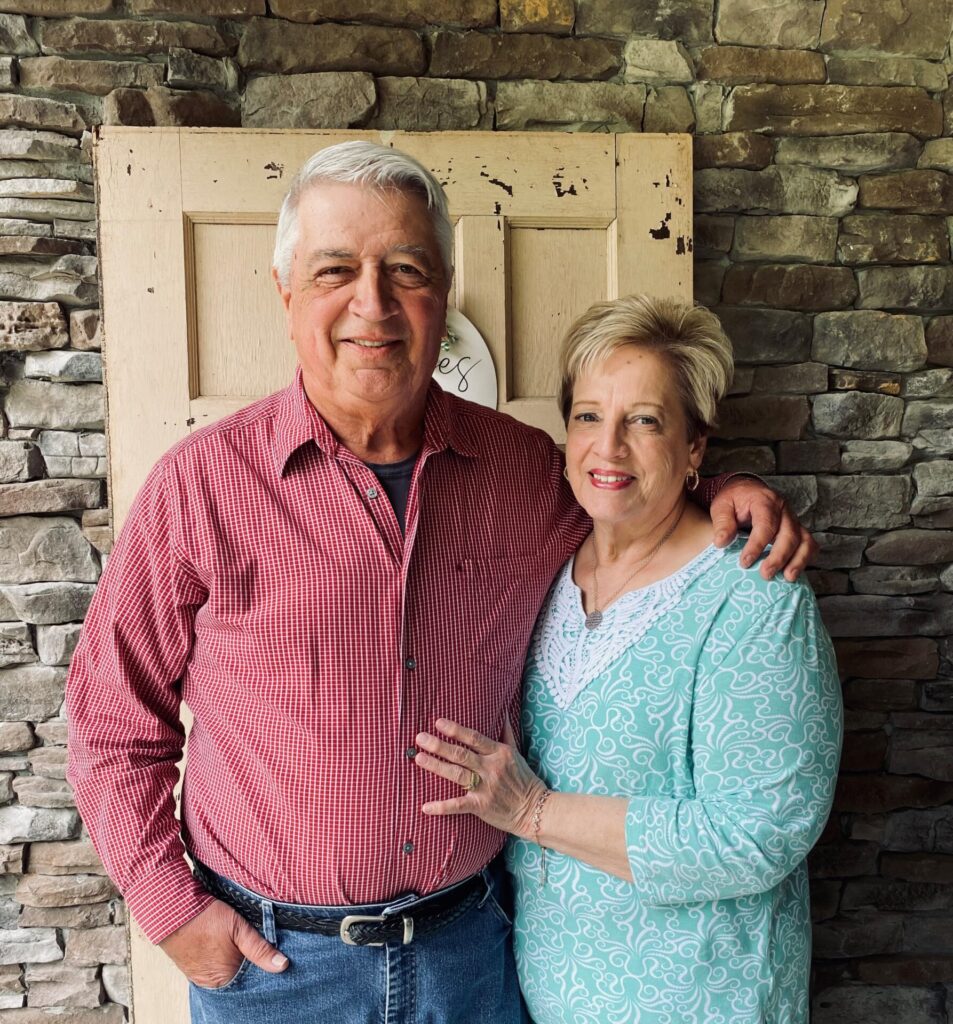
Chet Ramsey Receives Covenant Health’s Buscetta Award

Chester R. “Chet” Ramsey, Ph.D., director of medical physics at Thompson Cancer Survival Center, has been named winner of the 2015 Buscetta Award, given to outstanding managers within Covenant Health who personify leadership excellence. The award was presented by Covenant Health President and CEO Tony Spezia.
“It is with deepest appreciation that I express my thanks for being chosen as a recipient of the 2015 Buscetta Leadership Award,” Ramsey said. “Since joining Covenant Health, I have wanted to help cancer patients in our community. I feel that receiving the Buscetta Leadership Award is a tribute to the entire oncology team at Covenant Health, who are making a difference in the lives of cancer patients every day.”
Nominations for the fourth annual award were submitted by Covenant Health’s senior leaders. The award is named for Sam Buscetta, retired executive vice president for human resources, who was instrumental in launching Covenant Health’s Journey to Excellence initiative. Buscetta and his wife, Judy, were special guests at the award presentation and a luncheon for honorees.
Nominees were evaluated in areas such as quality, service, growth, finance/cost management and developing people, along with achievements related to systemwide alignment and innovation. In announcing the 11 award finalists from throughout Covenant Health, Spezia said they represented “the very best of Covenant Health’s leadership.”
As the health system’s chief medical physicist, Ramsey is “the internal expert for radiation oncology matters,” said Ann Henderlight, chief nursing officer at TCSC, during her introduction of Ramsey as a nominee. “He is the go-to person for identification, evaluation and installation of technology for radiation oncology and PET/CT across the system,” she said. In his role, Ramsey is proactive in referral development and a connector for all cancer centers in Covenant Health.
In congratulating the nominees, Spezia noted that “many of our managers and directors have been promoted to leadership roles after serving on the front lines of caring for patients, providing ancillary services, or making sure that our technology and other support systems are working efficiently.
“Buscetta award nominees have an understanding of how our hospitals and facilities function, and often work shoulder-to-shoulder with their colleagues to help their departments run smoothly. In addition, they are often mentors, advisors, and confidantes. These strong managers and directors are absolutely critical to Covenant Health.”
In addition to Ramsey, congratulations to these 2015 Buscetta Award finalists:
- Becky Baldwin, director of patient registration & financial services, Methodist Medical Center
- Carol Burns, director of patient registration & financial services, Fort Sanders Regional Medical Center
- Michelle Dalton, director of pharmacy, Morristown-Hamblen Healthcare System
- Miles Denton, director, food and nutrition services, LeConte Medical Center
- Karyn Goins, manager, cardiopulmonary, Fort Loudoun Medical Center
- Sandy Gragg, director of pharmacy, Roane Medical Center
- Chris Hall, manager, lab services, Fort Snaders Regional
- Bernie Hurst, director, women’s services and medical/surgical nursing, FSRMC
- Kristi Ramage, nurse manager, surgery services, LeConte Medical Center
- Connie Wagner, director of radiology, Parkwest Medical Center and Peninsula, a Division of Parkwest
[bs_row class=”row”][bs_col class=”col-sm-6″]

[/bs_col][bs_col class=”col-sm-6″]

[/bs_col][/bs_row]
[bs_row class=”row”][bs_col class=”col-sm-12″]

[/bs_col][/bs_row]